Benefits verification

Benefits verification is more complex than ever
The type of “out-of-network” coverage insurance companies stipulate determines the way doctors are reimbursed.
Wait times for health insurance eligibility verification can vary from ten minutes to several hours. And even then, it can still be inaccurate or incomplete.
Keeping up with the constant changes in third-party payment can put significant strain on your office staff.

How it works
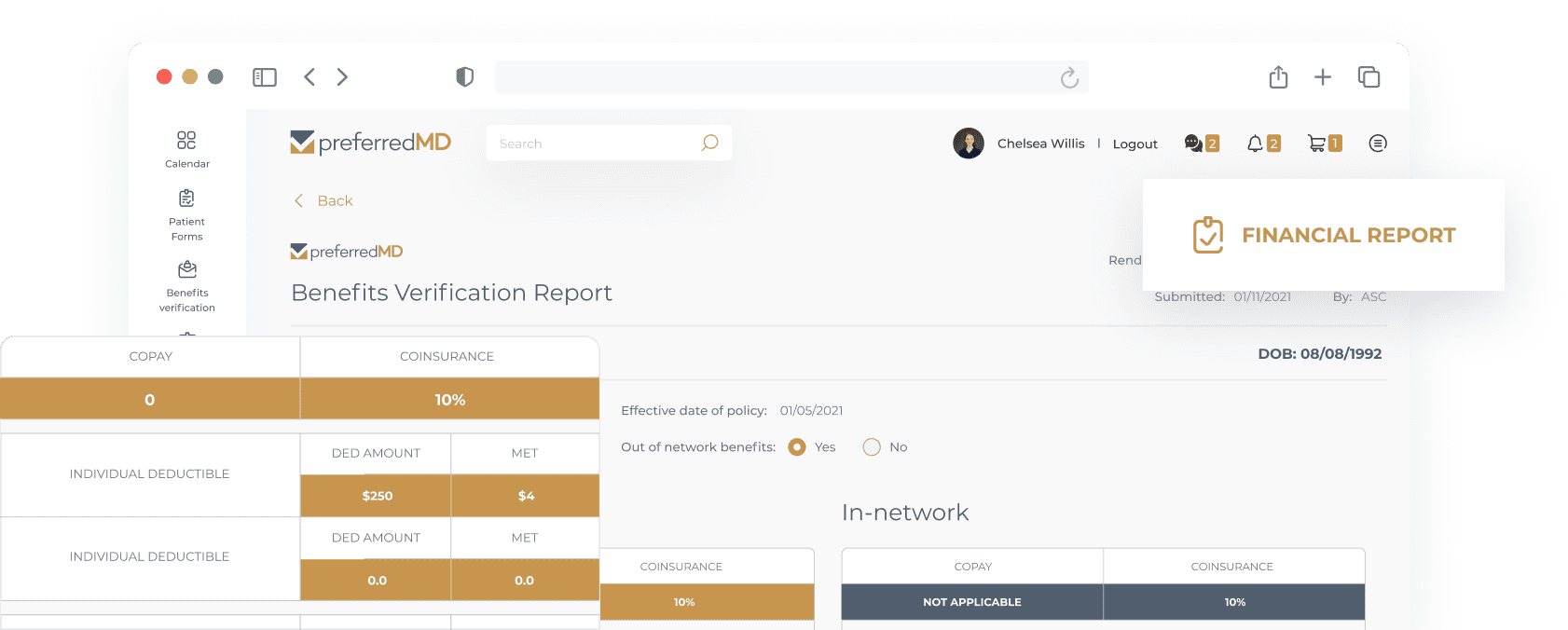
To initiate a request, you upload patient demographics and insurance information to the PreferredMD health insurance benefits verification portal.
We review the information, contact the insurance company, and verify the fee schedule.
Our Quality Assurance team thoroughly reviews each report to make sure it’s accurate and complete.
If there are no complications beyond our control, most requests are handled within 24 hours.





Outsource insurance benefits verification to PreferredMD – you’ll be glad you did
Join the premier out-of-network health insurance verification service and pay a low flat fee of just $20 per request. No setup or onboarding fees.
Get timely, detailed information in our easy-to-read benefits verification reports you can upload into the patient’s chart within hours of the request, along with a reimbursement schedule.
Improve patient interactions and collections and reduce the amount of billing that ages and ultimately becomes uncollectible.

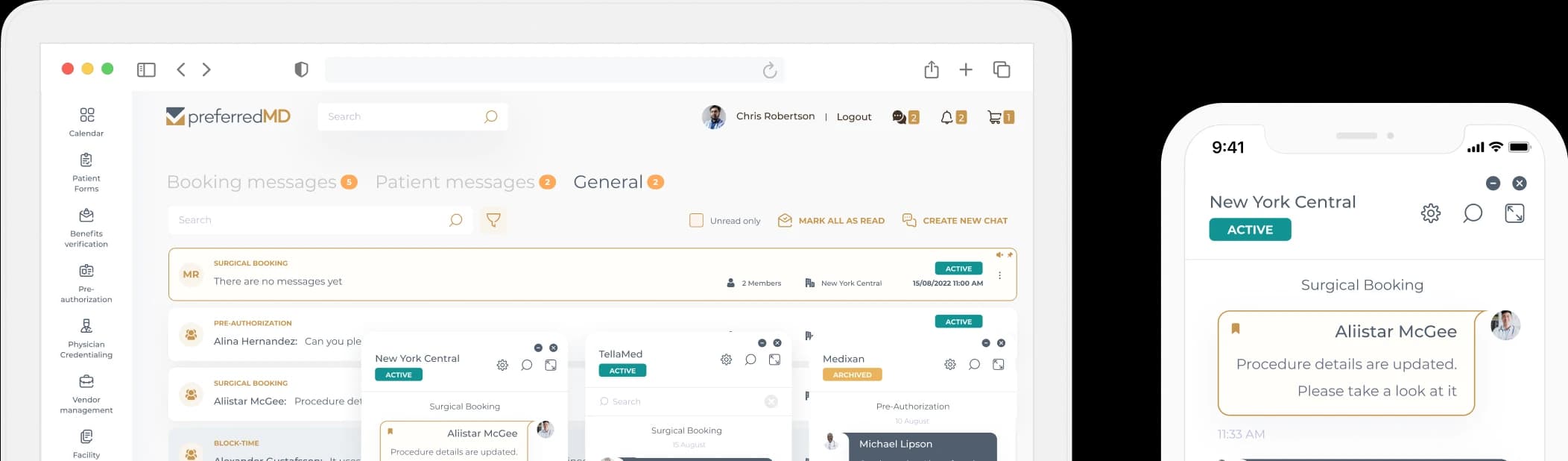
Streamline all processes with one easy-to use digital platform for physicians and facilities
Surgical Scheduling
Vendor management
Physician credentialing
See how others already benefit from PreferredMD
Ready to reduce your operating expenses with PreferredMD?
Schedule a demo in one click
Schedule a demo